Radiation Treatment Program Timeline – 2009 to 2023

2009 Reporting radiation wait times to the public
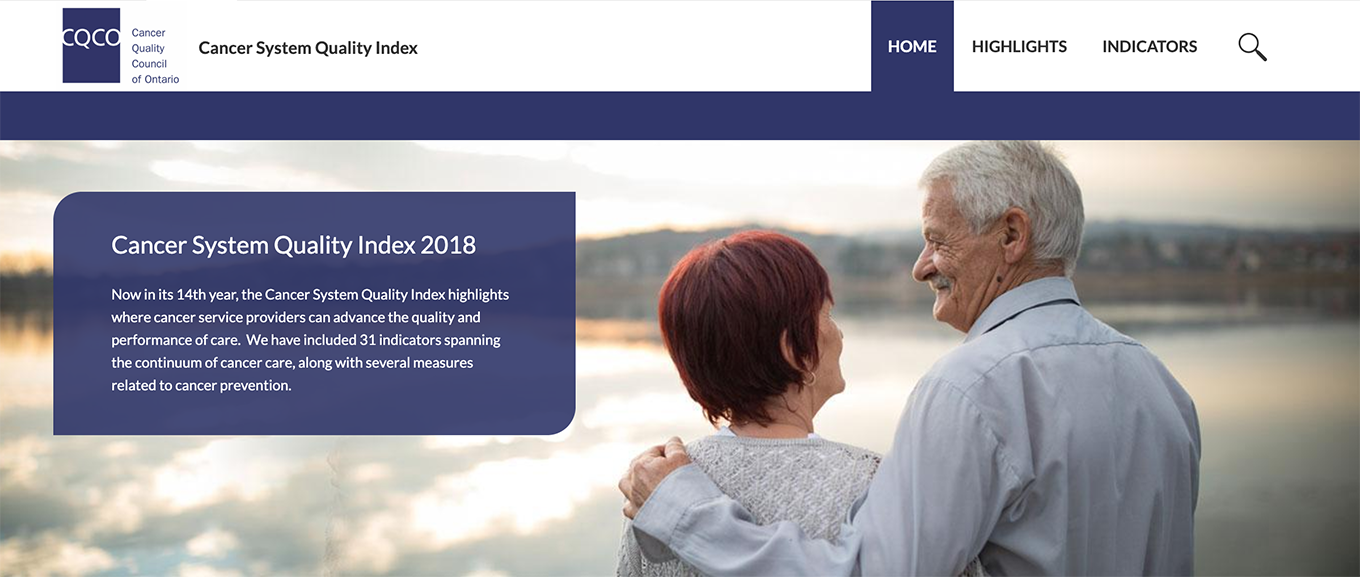
Cancer Care Ontario has been reporting wait times publicly, by cancer centre and type of cancer, since 2004. More recently, the Cancer System Quality Index started reporting integrated radiation treatment wait times for head and neck and cervical cancers.
Establishing a new role: clinical specialist radiation therapist
Between 2009 and 2016, radiation treatment teams across the province added clinical specialist radiation therapists to their teams. This new role increases capacity, improves quality of care and ultimately improves the health of Ontarians.
The Radiation Treatment Program has been supporting the development of this new model of care since 2004 with the clinical specialist radiation therapist project
 Play video – CSRT: An Innovative Model of Care
Play video – CSRT: An Innovative Model of Care
Collecting information about radiation incidents across the province
We began reviewing provincial radiation incident rates quarterly safety teleconferences. The data helped us analyze trends, and facilitated discussion to improve safety. Information about serious incidents is quickly passed on to the cancer centres.
Thanks to a collaboration with the Canadian Institute for Health Information, the Canadian Partnership for Quality in Radiotherapy, and our regional partners, Ontario radiation incident data is now reported at a national level.
Implementing intensity-modulated radiation therapy across Ontario
Intensity-modulated radiation therapy (IMRT) is an advanced way to deliver high doses of radiation to cancerous tumours with less damage to surrounding healthy tissues. In 2009, the Ministry of Health and Long-Term Care funded a 3-year project to put this treatment in place across the province as the standard of care for all eligible Ontarians.
As part of this project, we:
- co-developed and published organizational guidelines for 10 disease sites with the Program in Evidence-Based Care
- coordinated training and education for 825 radiation treatment professionals
- provided coaching for clinicians at the regional cancer programs
- produced several publications
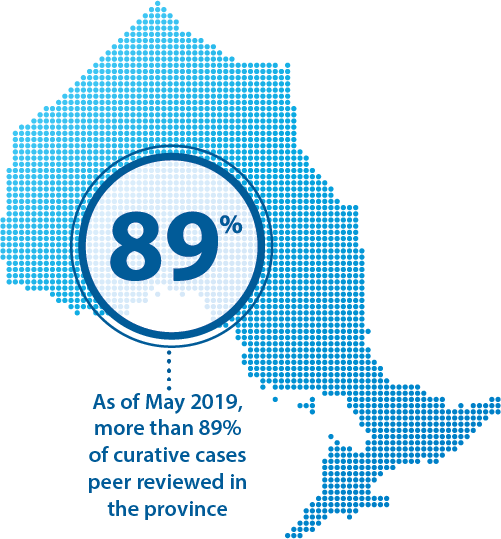
2011 Implementing provincial peer review quality assurance in radiation treatment
The Peer Review Quality Assurance initiative, begun in 2011, supports and facilitates peer review across cancer centres in Ontario. As of fiscal year 2018/2019, more than 80% of curative cases and above 50% of palliative cases (complex and non complex) are peer reviewed in the regional cancer centres.
The peer review team also works with the Canadian Partnership Against Cancer to develop national best practices, by type of cancer, for peer review of specific types of radiation treatments. As of 2019, best practices are in place for breast and lung cancers.
2012 Developing provincial communities of practice
When the regional cancer centres transferred from Cancer Care Ontario to hospitals, the regional radiation therapy departments lost a regular point of contact. We developed a communities of practice program to help re-build connections among the provincial radiation treatment community.
The communities of practice promote collaboration among cancer centres with a goal to decrease variation in practice and improve patient care. Community of practice leaders – volunteer, front-line healthcare professionals – identify and prioritize quality issues and choose projects to carry out.
The communities of practice have been successful in knowledge creation, knowledge transfer and exchange, and community building.

Helping Ontarians access proton therapy
Proton beam therapy uses protons instead of X-rays to treat cancer with radiation. Proton therapy reduces radiation delivered in the normal tissue around the tumour.
Increasing evidence supports proton therapy over conventional radiation treatment for some groups of cancer patients. Proton therapy is especially important for children and young adults with brain tumours, and for the treatment of some cancers in adults.
Canada does not have a hospital-based proton beam therapy facility. That means people with cancer and their families must travel to the United States to receive this treatment.
We work with Cancer Care Ontario’s Out-of-Country Program to provide faster access for Ontarians who would benefit from this treatment. We also supported hospitals to develop and present a funding proposal to the Ministry of Health to assess the need for a proton beam radiotherapy facility in Ontario.

2016 Providing annual reports of radiation utilization data, by hospital of diagnosis, to regional cancer centres
One-year radiation treatment utilization in Ontario measures the proportion of patients diagnosed with a first cancer who have radiotherapy within 1 year of diagnosis.
The provincial utilization rate for 2015/16 was 34.1% – a 3.9% shortfall from the provincial benchmark of 35.5%. This means about 860 patients who may have benefited from radiation treatment that year did not receive it.
The Radiation Treatment Capital Investment Strategy 2018 aims to make sure Ontario has enough radiation capacity to reach the target rate. However, increased capacity alone will not ensure that people who would benefit from radiation therapy actually receive it. Other considerations include educating referring physicians, providing care closer to home and providing accommodation for patients who would have to travel to a radiation facility away from home to receive care.
Data about radiation utilization is reported every year in the Cancer System Quality Index.
Implementing a regional approach for magnetic resonance imaging guided brachytherapy for locally advanced cervical cancer patients
With the Gynecological Cancers Community of Practice, we developed and partially implemented a new treatment approach for people with locally advanced cervical cancer. Magnetic resonance imaging-guided brachytherapy uses the high-quality images of MRI to help with brachytherapy needle placement. Compared with traditional treatment approaches, this is linked with:
- lower rates of cancer recurrence
- better overall survival
- fewer complications
Since 2016 we have:
- Partnered with the Program in Evidence-Based Care to develop a guidance document on magnetic resonance guided brachytherapy over traditional treatment approaches
- Collaborated with Ontario health economist experts at the Centre for Excellence for Economic Analysis Research, St. Michael’s Hospital, to:
- assess the cost-effectiveness (utility?) of the new treatment technique compared with traditional approaches
- estimate the incremental cost of making this technique available to all women in Ontario

2017 Introduction of patient and family advisors into the Radiation Treatment Program
We brought 2 patient and family advisors on board to participate and advise on Radiation Treatment Program projects. They bring invaluable patient experience and perspective to the provincial planning and operation of radiation services in Ontario. The patient and family advisors supported the development of the Radiation Treatment Capital Investment Strategy 2018 and the Radiation Treatment Program Strategic Plan 2019 to 2023.

2018 Supporting the Radiation Treatment Capital Investment Strategy 2018
Radiation Treatment Program supported capital investment planning for Ontario in collaboration with the Systems and Infrastructure Planning team at CCO. This work led to a 45% increase in radiation machine capacity in the province over the past 13 years. The number of radiation treatment machines increased from 74 in 2005 to 107 in 2018. For details, see the Radiation Treatment Capital Investment Strategy 2018.
Developing a new funding model for radiation treatment services
We are developing a new funding model, in collaboration with CCO’s Funding Unit. The new funding model will drive consistent, equitable and high-quality care for radiation treatment services in Ontario. With the quality-based procedures funding model, the funding follows the patient. This model also promotes sharing best practices to improve quality, system efficiency and evidence-based care.
2022 Implementation of funding model for radiation treatment services
The Radiation Treatment Quality Based Procedures improves the use of resources in Ontario by tying funding to specific patient care activities. The development of the model supports the sharing of best practices between regional cancer centres, the identification of key quality metrics, and ultimately supports the adoption of a more standardized approach to care for patients.

2023 Implementation of Biodegradable Rectal Spacers for Prostate Cancer Radiotherapy
The Radiation Treatment Program launched the Rectal Spacer Reimbursement Program which included a Special Access Program. The program funds rectal spacers for eligible prostate cancer patients which reduces rectal toxicity during radiotherapy. It isa cost-effective option that has a clinically significant improvement in the quality of life for patients. The launch of the program included creation of an expert panel to develop clinical guidance, new operational processes and policies, data collection and communication resources for regional stakeholders.