Radiation Treatment Program
Implementation Plan 2019–2023

A companion report to the Ontario Cancer Plan
Notice of Extension: Radiation Treatment Program
Download a copy of the 2023-2024 implementation plan below
This first Radiation Treatment Program implementation plan is based on the Ontario Cancer Plan 2019 to 2023. This plan identifies program areas of focus for the next 4 years to support safe, accessible, high-quality radiation treatment for all Ontarians.
The goals of the implementation plan are to ensure that:
- all people who need radiation treatment get safe, appropriate high-quality care based on the best available evidence
- barriers to access care are actively addressed so patients who would benefit from radiation treatment can receive it as close as possible to home
- innovative radiation treatment approaches are evaluated and adopted in a timely way
This plan was developed in consultation with clinicians, administrators, regional partners, and with input from patient and family advisors across the province. Through continued collaboration with these groups, and, in time, Ontario Health[*], we can work through the initiatives in this plan to achieve the goals of the Ontario Cancer Plan and improve the performance of our health systems.
Padraig Warde
Provincial Head of Radiation Treatment
“The Radiation Treatment Program Implementation Plan describes our plan to work across 5 strategic areas of focus to continue to improve and support delivery of the highest quality of care for patients every step of the way through their treatment journey, while putting patients at the centre of every decision we make and everything we do.”
Robin McLeod
Vice-President, Clinical Programs & Quality Initiatives
“Radiation is a common and effective treatment modality for cancer patients. In Ontario, patients can be assured that they receive safe and effective cancer treatment, as well as patient-oriented care. This implementation plan will guide care for patients who require radiation for the next 4 years. It will ensure that patients continue to receive the best treatment, and that new treatments and innovations are adopted as they are developed.
Ontario has been a leader in the introduction of peer review – a process where a second radiation oncologist reviews the plan to ensure that patients receive the correct treatment – and this will be implemented in other aspects of radiation. We will continue to ensure that patients receive new and innovative care, and that care is provided in a timely way. We will also adopt a new funding model tied to best practice care. All of these initiatives will lead to improved patient care.
The implementation plan was developed by the Radiation Treatment Program team at Cancer Care Ontario, led by Dr. Padraig Warde. In addition, multiple stakeholders, and patients and family members provided input. I thank all of them for contributing to this important work.”
Program Areas of Focus
This implementation plan deals with issues beyond capital planning, which was the Radiation Treatment Program’s main focus in the past. All of these areas of focus support the “Person-Centred” goal from the Ontario Cancer Plan 2019 to 2023, and align with a corresponding strategic objective.
To learn more about the program’s work to improve the quality of radiation treatment in Ontario over the past 10 years, view the Radiation Treatment Program Timeline
These are our 5 areas of focus for the next 4 years:
Radiation Treatment in Ontario
Current state
The Radiation Treatment Program works closely with the Surgical Oncology, Systemic Treatment, Psychosocial Oncology and Palliative Care Programs to provide an integrated cancer treatment approach for people with cancer in Ontario.
After a person is diagnosed with cancer, their treatment options are determined by the type and extent of the disease, and their individual needs and preferences. For many people with localized cancers that can be cured, radiation therapy is an essential element of their treatment plan. It also can lessen symptoms for many people with cancer that is locally advanced or has spread to other parts of the body.
In Ontario, radiation services are offered only in the 14 regional cancer centers and 3 satellite radiation treatment facilities. Since the patient management, radiotherapy treatments, and the capital infrastructure required to support a radiation medicine program are highly specialized, some degree of treatment centralization is required to ensure high quality of radiotherapy services.
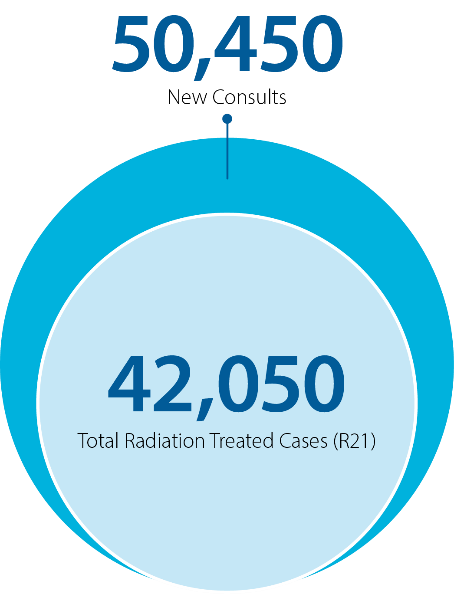
In 2018, over 50,000 newly diagnosed patients were assessed for radiation treatment; over 42,000 of those patients received treatment (see figure). More than 25% of patients who had radiation treatment intended to cure their cancer also had chemotherapy at the same time to make the tumour more sensitive to the effects of radiation treatment.
Number of patient consults and treated cases
Looking to the future
Cancer is one of the leading causes of death worldwide, with an estimated 18.1 million cases and 9.6 million deaths in 2018.[12] One in every 2 Ontarians is expected to be diagnosed with cancer during their lifetime.[13] The number of new cancer cases diagnosed each year in Ontario continues to increase. Approximately 90,500 new cases of cancer were diagnosed in Ontario in 2018. That is about 571 cases of cancer for every 100,000 people (after adjusting for age).[13]
NEW CANCER CASES ARE RISING
DEMAND FOR RADIATION TREATMENT IS GROWING
As the number of new cases of cancer and access (utilization rates) to treatment improves, the demand for radiation treatment continues to grow. The number of people treated with radiation has grown from 37,136 in 2012 to 42,060 in 2018, about 2% each year. As the population grows and ages, the number of newly diagnosed cancers is expected to rise by approximately 4% annually over the next 10 years.[14]
This increased demand will place pressure on the system, including on radiation medicine programs across Ontario as the need for health human resources increases. In addition, with improved systemic treatments and technologies for cancer, many patients are living longer and receiving an increased number of palliative radiation therapy courses than in the past.
The Radiation Treatment Capital Investment Strategy 2018 identifies the need for an additional 26 treatment units by 2028 to assure appropriate access to care.
“When I was diagnosed with breast cancer, I received my radiation treatments at The Ottawa Hospital, 20 minutes away from my home. But a friend of mine in North Bay who also had breast cancer had to travel to Sudbury for her radiation. That meant she had to stay in Sudbury, away from her husband and children, for a week at a time. Having cancer is the biggest stress in your life. You shouldn’t have to travel long distances or be away from your supports.”
For more information
RADIATION TREATMENT PROGRAM
Learn about the program’s work in improving access to treatment, capacity planning, quality improvement and evaluation of new technologies.
CAPITAL INVESTMENT STRATEGY
Find a detailed description of Ontario’s capital investment needs for radiation treatment for the next 10 years.
Evaluating our Progress
The Radiation Treatment Program Implementation Plan will be evaluated using the Realist Evaluation Framework (Pawson & Tilley, 1997). This framework accommodates changes and unknown variables that may develop during implementation. It provides a practice iterative and tailored approach to guide the evaluation of the plan.
The program will test the identified areas of focus over the next 4 years by evaluating the outcomes and adapting the initiatives as needed.
Realist Evaluation Framework
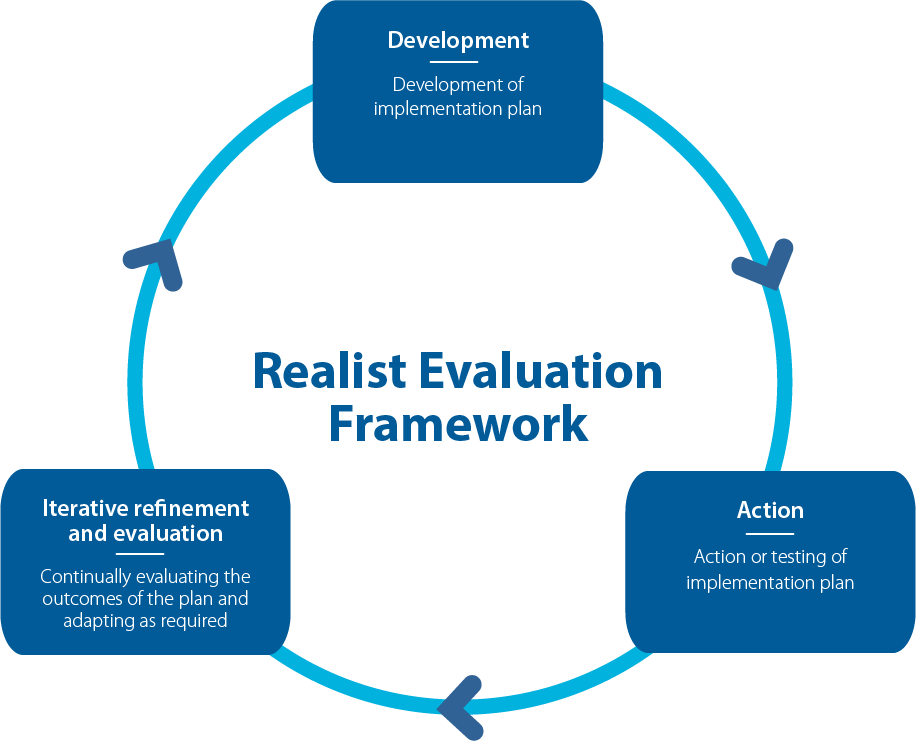
How this plan uses the framework
The implementation and evaluation of the initiatives will depend on the following questions:
- What mechanisms will generate the desired outcomes?
- What features of the context will affect if or how the mechanism operates?
The following table describes how the program will measure the successful implementation of the areas of focus and respective initiatives.
| Program Area of Focus | Outcome Measure | Description |
|---|---|---|
| Radiation Integrated Wait Time | Reduction in wait times from referral to radiation oncology to start of treatment | Improve the patient’s wait time experience from referral to radiation oncology to the date of first treatment |
| New Funding Model | Ongoing monitoring of quality metrics through regular reporting, surveys and chart audits | Develop and implement a new funding model that provides best practice and equitable care for all patients |
| Access/Utilization | Improved access to state of-the-art care for all Ontarians | Achieve sustained improvement in access to radiation treatment for patients in all healthcare regions across the province |
| Peer Review | Improved quality and safety of radiation treatment | Provide safer and higher quality radiation treatment for patients and across cancer centres |
| Supporting Innovative Treatment Approaches | Enable rapid clinical, operational and financial assessment of innovative techniques | Support dissemination of innovative treatment approaches, where appropriate, in a timely way to Ontario patients |
About This Plan
Methodology
The Radiation Treatment Program Implementation Plan was developed during 2018 and 2019. This iterative process included:
- initial planning, data gathering and analysis in consultation with clinicians and administrators
- review of related strategic plans on a regional, national and international level
- ongoing consultation with stakeholders throughout the province as the plan was refined, including patient and family advisors, regional cancer centres and other CCO business areas
- review of and reflection on the Radiation Treatment Program’s successes (and failures) over the past decade
The Radiation Treatment Program Implementation Plan aligns with the capital investment strategy, which supports:
- maintenance and improvements in radiation therapy wait times
- radiation therapy replacement grants
- utilization rates
- capacity planning
Partners
Thank you to the partners at the regional cancer centres for their invaluable support. Their commitment and support is critical to this program’s success in improving care for people with cancer in Ontario.
- Regional radiation clinical leads
- Professional advisory committees: radiation oncology, medical physics, radiation therapy
- Community of practice members, working group leads, and leads
Acknowledgements
The following CCO staff, advisors and volunteers contributed to this plan.
EXECUTIVE SPONSORS
Garth Matheson, Vice-President, Planning and Regional Programs, and Analytics and Informatics
Robin McLeod, Vice-President, Clinical Programs and Quality Initiatives
CLINICAL PROGRAMS & QUALITY INITIATIVES
Padraig Warde, Provincial Head, Radiation Treatment Program
Elaine Meertens, Director, Diagnosis and Treatment Programs
Eric Gutierrez, Group Manager, Radiation Treatment Program
Farzana McCallum, Team Lead, Radiation Treatment Program
Carina Simniceanu, Senior Specialist, Radiation Treatment Program
Julie Himmelman, Senior Specialist, Radiation Treatment Program
RADIATION TREATMENT PROGRAM CLINICAL QUALITY LEADS
Michael Brundage, Radiation Oncologist
Margaret Hart, Radiation Therapist
Jean-Pierre Bissonnette, Medical Physicist
OTHER CONTRIBUTORS AND PARTNERS
Sophie Foxcroft, Systems and Infrastructure Planning
Jon Irish, Provincial Head of Surgical Oncology Program
Leta Forbes, Provincial Head of Systemic Therapy Program
Claire Holloway, Provincial Clinical Lead, Disease Pathway Management
Julian Debranowski, Program Head, Imaging
Alethea Kewayosh, Director, Indigenous Cancer Care Unit
Joanne MacPhail, Patient and Family Advisor
Derek Finnerty, Patient and Family Advisor
Ann Rawson, Patient and Family Advisor
References
- Chung J, Ju G, Yang J, Jeong J, Jeong Y, Choi MK, Kwon J, Lee KH, Kim ST, Han HS. Prevalence of and factors associated with anxiety and depression in Korean patients with newly diagnosed advanced gastrointestinal cancer. The Korean journal of internal medicine. 2018 May;33(3):585.
- Graboyes EM, Kompelli AR, Neskey DM, Brennan E, Nguyen S, Sterba KR, Warren GW, Hughes-Halbert C, Nussenbaum B, Day TA. Association of treatment delays with survival for patients with head and neck cancer: a systematic review. JAMA Otolaryngology–Head & Neck Surgery. 2019 Feb 1;145(2):166-77.
- Neal RD, Tharmanathan P, France B, Din NU, Cotton S, Fallon-Ferguson J, Hamilton W, Hendry A, Hendry M, Lewis R, Macleod U. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. British journal of cancer. 2015 Mar 3;112(s1):S92.
- Song H, Fang F, Valdimarsdóttir U, Lu D, Andersson TM, Hultman C, Ye W, Lundell L, Johansson J, Nilsson M, Lindblad M. Waiting time for cancer treatment and mental health among patients with newly diagnosed esophageal or gastric cancer: a nationwide cohort study. BMC cancer. 2017 Dec;17(1):2.
- World Health Organization. Cancer Early Diagnosis. [Internet] [Publisher unknown]: Cancer Early Diagnosis; [date unknown] [cited 2019 Aug 30]. Available from: https://www.who.int/cancer/prevention/diagnosis-screening/en/
- Ontario Ministry of Health and Long-Term Care. Health System Funding Reform Frequently Asked Questions [Internet] [Publisher unknown]: Health System Funding Reform Frequently Asked Questions; [2013 Dec 30] [cited 2019 Aug 30]. Available from: http://www.health.gov.on.ca/en/pro/programs/ecfa/funding/hs_funding_qa.aspx#1
- Brundage, M., Dr., Kong, W., Hartman, M., Gutierrez, E., Zaffino, E., Simniceanu, C., . . . Warde, P., Dr. (n.d.). Report on the Use of Radiotherapy in Ontario (2015-2016), with particular reference to LHINs (2018 ed., Vol. Winter).
- World Health Organization, Radiotherapy Risk Profile − Technical Manual [Internet]. Geneva: WHO Press; 2008 [cited 2019 Aug 30]. Available from: https://www.who.int/patientsafety/activities/technical/radiotherapy_risk_profile.pdf
- Canadian Partnership for Quality Radiotherapy, Quality Assurance Guidelines for Canadian Radiation Treatment Programs [Internet]. Canadian Partnership for Quality Radiotherapy; 2015 [cited 2019 Aug 30]. Available from: http://www.cpqr.ca/wp-content/uploads/2013/09/QRT2015-12-03.pdf
- Cancer Care Ontario, Radiation Oncology Peer Review Guidance Document [Internet]. Cancer Care Ontario; 2013 [cited 2019 Aug 30]. Available from: https://www.cancercareontario.ca/sites/ccocancercare/files/assets/CCORadiationOncologyPeerReview.pdf
- Caissie A, Rouette J, Jugpal P, Davis CA, Hollenhorst H, O’Donnell J, Mitera G, Brundage MD, Pan-Canadian Peer Review Steering Committee. A pan-Canadian survey of peer review practices in radiation oncology. Practical radiation oncology. 2016 Sep 1;6(5):342-51.
- World Health Organization, International Agency for Research on Cancer, Cancer Today [Internet]. Geneva: WHO Press; 2008 [cited 2019 Aug 30]. Available from: https://gco.iarc.fr/today/data/factsheets/populations/900-world-fact-sheets.pdf
- Cancer Care Ontario, Clinical Specialist Radiation Therapist Project [Internet]. Cancer Care Ontario; [date unknown] [cited 2019 Aug 30]. Available from: https://www.cancercareontario.ca/en/cancer-care-ontario/programs/clinical-services/patient-reported-outcomes-symptom-management/radiation-treatment/clinical-specialist-radiation-therapist
- Cancer Care Ontario, Radiation Treatment Capital Investment Strategy [Internet]. Toronto: Cancer Care Ontario; 2018 [cited 2019 Aug 30]. Available from: https://www.cancercareontario.ca/en/programs/regional-cancer-programs/capital-investment-strategy




