The main cause of cervical cancer is human papillomavirus (HPV). HPV is a virus that is passed from one person to another through sexual contact. Sexual contact is when someone has contact with another person’s genitals (private parts). This contact can be with the hand, mouth or genitals. Learn more about HPV on the Cervical Screening page.
There are several things you can do to lower your risk of cervical cancer:
Consider HPV Vaccination
The HPV vaccine (Gardasil®) is available at no charge to all Grade 7 students through Ontario’s publicly funded school-based program.
People who do not qualify for the publicly funded school-based program can pay to get the HPV vaccine. If you are a person with a cervix, speak to your doctor, nurse practitioner or midwife about getting the vaccine.
It is best to have the vaccination before you have sexual contact with another person. But even if you have already had sexual contact with another person, you may benefit from the vaccine. The vaccine prevents most, but not all, cervical cancers.
Go for Regular Cervical Screening Tests
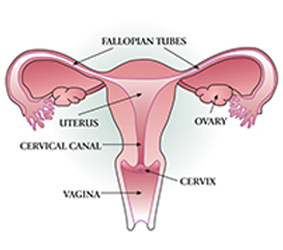
The cervical screening test checks for the types of HPV that can sometimes cause cervical cancer. It also checks for cell changes in the cervix caused by these types of HPV.
The cervical screening test has replaced the Pap test because it is better at helping prevent cervical cancer.
Regular screening with the cervical screening test is the best way to lower your chance of getting cervical cancer. Be sure to go for regular cervical screening tests and for more testing after an abnormal test result, if needed.
See the Screening section to find out more, including who should get cervical screening.
Do Not Smoke
The chance of getting cervical cancer increases by up to 80% for someone who is infected with a cancer-causing type of HPV if they also smoke. Smoking weakens the immune system, making it harder for the body to fight off an infection. Smoking is linked to many types of cancer and other diseases. There is no safe kind of commercial tobacco product and no safe amount of smoking.
It is never too late to benefit from quitting smoking. If you are already a non-smoker, keep yourself safe by avoiding other people’s tobacco smoke (second-hand smoke).
If you currently smoke tobacco, take some time to plan to quit smoking. Research suggests that a combination of counselling and medication will give you the best chance at being successful if you try to quit.
For more information about quitting smoking, you can visit the Canadian Cancer Society.
Reduce Your Chance of Getting HPV
80% of people will get HPV at least once in their lifetime. Your chance of being infected with HPV starts as soon as you have sexual contact and goes up with every new sexual partner. Your chance of being infected may also go up if a sexual partner is infected with HPV.
Some research shows that using condoms regularly can help lower the chance of getting cervical cancer because it lowers the chance of getting HPV. But condoms cannot fully protect against HPV or completely prevent cervical cancer.