There are several things you can do to lower your risk of melanoma:
Be Safe in the Sun
The most important risk factor for melanoma and non-melanoma skin cancer is exposure to ultraviolet (UV) radiation. People who spend a lot of time in the sun are more likely to get melanoma than people who spend little time in the sun.
Studies have shown that frequent sunburns – even if they happened years ago when you were a child or teenager – raise the risk of melanoma.
People who don’t tan easily in the sun or who have fair-coloured skin or light-coloured eyes are more likely to get UV radiation damage. Although melanoma is somewhat rare among people with very dark skin, they are not immune. Melanoma can happen in people with darker skin and may be harder to find early. Even if your natural skin colour is dark, it’s important to protect yourself from UV radiation.
No sunscreen can protect you 100% from UV radiation. Always use sunscreen, and wear protective clothing or find shade.
Don’t Use Tanning Beds or Sunlamps
Tanning equipment like tanning beds or lamps give off the same damaging UVA and UVB rays as the sun. As a result, people who use tanning equipment have at least a 20% increased risk of melanoma.
In Ontario, the Skin Cancer Prevention Act (Tanning Beds), 2013 banned the sale and marketing of tanning services to people under 18 years of age.
Know Your Skin
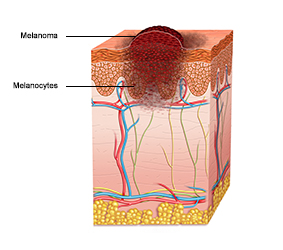
It’s important to know your skin. Check your skin regularly to look for warning signs such as:
- change in the shape, colour, size or surface of a birthmark or mole
- a sore that doesn’t heal
- any patch of skin that bleeds, oozes, swells, itches or becomes red and bumpy
It’s a good idea to check your moles regularly so you will know if they start to change. Use the ABCDE system to help you identify possible signs of melanoma:
- Asymmetry: if you were to draw a line through the mole or growth, the 2 halves wouldn’t match (e.g., one half is a different shape or colour than the other half).
- Borders: the edges are irregular, scalloped or notched.
- Colour: there may be a mixture of different colours, such as shades of tan, brown or black, or sometimes even white, red or blue within the same mole, sore, lump or growth.
- Diameter: keep an eye out for any spot that grows larger, particularly if it is bigger than 6 millimetres (about ¼ inch) in diameter.
- Evolving: the border, colour, elevation, shape or diameter changes or there is a new symptom such as bleeding, itching or crusting.
If you notice any change or new development, consult your doctor or nurse practitioner.
Be Aware of Products that Increase Sun Sensitivity
Some medications or products can make your skin more sensitive to the sun (photosensitivity). When you start a new prescription, over-the-counter medication or herbal remedy, read the product information and talk with your pharmacist. Ask if this product has been reported to make people more sensitive to the sun. If it has, you should be careful to protect yourself whenever you are in the sun.
Transplant patients have special sun protection needs. You can learn more at the Kidney Foundation of Canada.
Check If You Are High Risk
Examples of factors that may put you at higher than average risk include:
- a family history of melanoma, for example, a first-degree “blood” relative such as a mother, father, brother, sister or child with a history of melanoma
- a personal history of basal cell or squamous cell carcinoma of the skin (non-melanoma skin cancer)
- taking medications that weaken the body’s immune response (immunosuppressive therapy) or make skin more sensitive to the sun (photosensitivity)