Breast (Chest) Density Information for Healthcare Providers
The word "chest" is sometimes used when describing the breasts. Some people, including trans men, transmasculine people and nonbinary people, may prefer the term "chest". The term “breast” is still used to make sure the language is clear for everyone.
Learn how to access breast (chest) density information, risk factors for getting breast cancer, and recommendations for screening people with higher density. The content on this page is for family doctors, nurse practitioners and Ontario Breast Screening Program sites.
On This Page
- Breast Composition
- Reporting Breast (Chest) Density
- Defining Breast (Chest) Density
- Screening Intervals Based on Breast (Chest) Density
- How Ontario Breast Screening Program (OBSP) Participants Can Find Out Their Breast (Chest) Density
- High Breast (Chest) Density and Breast Cancer
- Information to Share with Participants About Breast (Chest) Density
- How Breast (Chest) Density May Change
Breast Composition
- Breasts contain 2 types of tissue: fatty and fibroglandular. Normal fibroglandular tissue appears dense (or white) on a mammogram, while fatty tissue appears non-dense (or black).
Reporting Breast (Chest) Density
- In the Ontario Breast Screening Program, breast (chest) density is determined from a mammogram and is interpreted by the reading radiologist using Breast Imaging Reporting and Data System (BI-RADS) breast density categories. BI-RADS is a visually estimated description of the volume of dense tissue on the mammogram[1] There are 4 BI-RADS categories: A, B, C and D (see Defining Breast [Chest] Density).
Defining Breast (Chest) Density
- Breast Imaging Reporting and Data System (BI-RADS) categories are visually estimated descriptions of the volume of dense breast (chest) tissue on a mammogram.[1] The categories provide clinicians with awareness of the limitations of mammography because they help indicate whether masses may be obscured by dense tissue. The sensitivity of mammography for non-calcified lesions decreases as the BI-RADS category increases.[1] If the reading radiologist finds that the breasts are not of equal density, the denser breast is used to categorize breast (chest) density.[1]
- There are 4 BI-RADS breast (chest) density categories. “BI-RADS A” indicates the least amount of dense tissue and “BI-RADS D” indicates the most amount of dense tissue:
- Category A – the breasts are almost entirely fatty
- Category B – there are scattered areas of fibroglandular density
- Category C – the breasts are heterogeneously dense, which may obscure small masses
- Category D – the breasts are extremely dense, which lowers the sensitivity of mammography
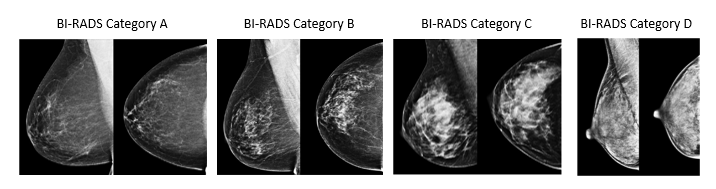
Mammographic images on pages 128-130 of the ACR BI-RADS® Atlas, 5th edition
Screening Intervals Based on Breast (Chest) Density
- Based on evidence, the Ontario Breast Screening Program (OBSP) recommends that participants with higher breast (chest) density (i.e., Breast Imaging Reporting and Data System [BI-RADS] D) be recalled for their next screening mammogram in 1 year.[2]
- A participant with a breast (chest) density result of BI-RADS A, B or C will be recalled for their next screening mammogram by the OBSP in 2 years if there are no other factors that would indicate a 1-year recall, such as family history of breast cancer.
- Participants who are concerned about their breast (chest) density and breast cancer risk can talk with their family doctor or nurse practitioner to discuss whether they have other risk factors (e.g., family history) that may increase their risk of getting breast cancer. They can also discuss ways to reduce their breast cancer risk (see Information to Share with Participants About Breast [Chest] Density).
How Ontario Breast Screening Program (OBSP) Participants Can Find out Their Breast (Chest) Density
- All OBSP screening mammogram reports contain a participant’s breast (chest) density measure in the form of a Breast Imaging Reporting and Data System (BI-RADS) breast (chest) density category. A family doctor or nurse practitioner will get a copy of their patient’s OBSP screening mammogram report from the OBSP site where the mammogram was performed.
- Ontario Health (Cancer Care Ontario) sends result letters to participants to notify them of normal mammogram results.
- As of July 2023, participants with a normal screening result will get their BI-RADS breast (chest) density result in their OBSP normal result letter, along with a Breast (Chest) Density Fact Sheet.
- If a participant has normal screening results and a breast (chest) density result of BI-RADS D, they will be notified that they will be recalled for screening in 1 year instead of 2 years due to dense breast tissue on their mammogram.
- We do not send participants a copy of their OBSP screening mammogram report. If a mammogram result is abnormal and more testing is needed, the OBSP site, family doctor or nurse practitioner will contact the participant directly.
- Since participants with abnormal screening results do not have direct access to breast (chest) density information, primary care providers will need to consider sharing breast (chest) density results with their patients at the appropriate point during follow up of their abnormal results.
- Participants without a family doctor or nurse practitioner can find out their density result by contacting their OBSP site for a copy of their OBSP screening mammogram report.
High Breast (Chest) Density and Breast Cancer
- Higher density relates to the risk of developing breast cancer for 2 reasons:
- Breast cancer and masses look white on a mammogram. Dense tissue also looks white, so it can be harder to find breast cancer on a mammogram if someone has high breast (chest) density.
- Research shows that the risk of breast cancer increases as the amount of dense tissue in the breast increases.[3]
- High density is one of several factors (e.g., BRCA1/2 gene mutations, personal history of breast cancer, physical inactivity) that can affect someone’s risk of developing breast cancer. In a study of screen-eligible populations that included Canadians ages 50 to 69 from Ontario and British Columbia, higher density was associated with a higher risk of developing breast cancer.[2]
Information to Share With Participants About Breast (Chest) Density
- Participants should be aware that the presence of dense breast (chest) tissue is normal and very common, and it is important to get regular mammograms.
- Participants cannot do much to change their density; however, it can be affected by other factors (see How Breast [Chest] Density May Change).
- Participants can visit cancercareontario.ca/breastdensity for information on density and risk factors for breast cancer.
- Although higher density may increase the risk of developing breast cancer, modifiable lifestyle choices may also affect the risk of developing breast cancer. These modifiable lifestyle choices can affect breast cancer risk more than high density.
- For information on modifiable breast cancer risk factors (e.g., alcohol consumption, adult weight gain and physical activity), please visit Risk factors you can change or control at mycanceriq.ca.
- For information on non-modifiable breast cancer risk factors (e.g., genetics), please visit Risk factors you can’t change or control at mycanceriq.ca.
How Breast (Chest) Density May Change
- Breast composition changes with age. For example, menopause causes estrogen levels to decrease and can cause breasts to become more fatty and less dense.[4]
- Some people have higher density after taking estrogen.
Supplemental Screening for People with Breast Imaging Reporting and Data System (BI-RADS) D Breast (Chest) Density
- One way to improve cancer detection in people with dense breasts is through supplemental screening, which involves screening with another type of imaging test in addition to mammography. Types of breast imaging tests that can be used for supplementary screening include ultrasound and magnetic resonance imaging.
- Evidence on the benefit of supplemental screening for breast cancer has been evolving. Ontario Health conducted a health technology assessment to review published evidence on the effectiveness and cost-effectiveness of supplemental screening. In December 2023, based on guidance from the Ontario Health Technology Advisory Committee, Ontario Health released a recommendation to the Ministry of Health to publicly fund supplemental breast cancer screening for people with BI-RADS D density. Ontario Health recommended publicly funding supplemental screening for people with BI-RADS D density, but not for people with BI-RADS densities A to C due to insufficient clinical evidence on the benefit of supplemental screening in these populations.
- Primary care providers may choose to discuss the benefits and risks of supplemental screening with their patients who have BI-RADS D density and refer them for supplemental screening outside of the OBSP. For example, the health technology assessment showed that the benefits of supplemental screening in people with dense breasts include improving cancer detection rates and reducing the likelihood of interval cancers, but its harms include higher abnormal recall rates and more people getting additional testing, such as breast biopsies. Read more about the recommendation and health technology assessment on the Health Quality Ontario supplemental screening page.
- The OBSP will continue to recall participants with BI-RADS D density for a screening mammogram one year after their last mammogram and will continue to recall these participants for regular screening regardless of whether they have had supplemental screening.
- Ontario Health plans to update the OBSP to include supplemental screening for people with BI-RADS D density based on the health technology assessment and expert panel input in the future.
