First Nations, Inuit, Métis and Urban Indigenous Cancer Strategy 2019–2023
Since 2004, multi-year provincial Indigenous[*] cancer strategies have addressed and led to improvements in cancer care for Indigenous people in Ontario. The First Nations, Inuit, Métis and Urban Indigenous Cancer Strategy 2019 – 2023 continues the work set out in the first 3 strategies.
This strategy provides a road map for how Ontario Health (Cancer Care Ontario),[*] Indigenous communities and individuals, and health system partners will work together to:
- improve the performance of the cancer system for Indigenous people in Ontario in a way that honours Indigenous concepts of well-being
- improve the well-being of Indigenous people in Ontario and reduce the burden of cancer in these communities
- empower supportive and healthy environments that build on the strengths of Indigenous individuals, families, communities and organizations
Community Voice
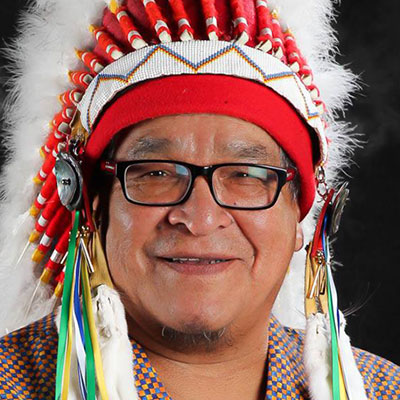
Glen Hare
Grand Council Chief, Anishinabek Nation

“We cannot forget that our people are suffering from a higher incidence of several types of cancer compared to other people in Ontario. Our people are continuing to die prematurely from certain preventable and treatable cancers. The important thing is prevention and getting screened to find cancer early, as opposed to trying to react when it is too late. We need to equip our Peoples with the information they need to take control of their health and well-being. ”
Glen Hare, Grand Council Chief, Anishinabek Nation
Alvin Fiddler
Grand Chief, Nishnawbe Aski Nation

“NAN First Nations face many challenges including lack of early diagnosis and access to related services due to remoteness and an inequitable healthcare system. By working with Cancer Care Ontario this strategy will allow us to develop effective planning for timely access and more effective screening and education in the delivery of cancer services in our communities.”
Alvin Fiddler, Grand Chief, Nishnawbe Aski Nation
Francis Kavanaugh
Ogichidaa (Grand Chief), Grand Council Treaty #3

“I am very pleased with the strong partnership between Grand Council Treaty #3 Health Council and Cancer Care Ontario. This partnership has yielded the Grand Council Treaty #3 cancer report, which was developed through significant direction from our Grand Council Treaty #3 Cancer Surveillance Advisory Team that consisted of our Grand Council Treaty #3 Health Council and several representatives from our communities. It will help us properly plan programs and support services. Together, we will continue to work towards understanding and improving the impact of cancer in our communities.”
Francis Kavanaugh, Ogichidaa (Grand Chief), Grand Council Treaty #3
Sylvia Maracle
Executive Director, Ontario Federation of Indigenous Friendship Centres
“The relationship between Cancer Care Ontario and the Ontario Friendship Centres stands as an example of how urban Indigenous organizations should be engaged in the healthcare system. When we each respect and support the pivotal role we each play in Indigenous health and well-being, we can make even greater strides to collectively reduce the burden of cancer on Indigenous people.”
Sylvia Maracle, Executive Director, Ontario Federation of Indigenous Friendship Centres
Jason LeBlanc
Executive Director, Tungasuvvingat Inuit
“Tungasuvvingat Inuit is pleased to continue to work in partnership with Cancer Care Ontario and ensure the voices and specific needs of Inuit and their families are represented throughout the cancer care system of Ontario. As we build upon our past successes, we see a future where Inuit are empowered in their own healthcare journeys and are able to support and influence the healthcare system to be inclusive and equitable for our people.”
Jason LeBlanc, Executive Director, Tungasuvvingat Inuit
Margaret Froh
President, Métis Nation of Ontario

“The Métis Nation of Ontario are proud of our ongoing collaboration with Cancer Care Ontario towards a healthier and increasingly empowered quality of life for Métis citizens and families in Ontario. The relationship we have forged together continues to build upon solid research, education and programming goals -- created by and for Métis -- that will ultimately allow our communities to better understand and address the complexities of cancer in their lives. We look forward to creating new and innovative initiatives under this strategy that will create greater awareness, support and prevention of cancer through a holistic lens unique to the Métis experience.”
Margaret Froh, President, Métis Nation of Ontario
Strategic Priorities, Objectives and Actions
Cancer in Indigenous Communities
Why Ontario needs an Indigenous cancer strategy
There is an urgent need for action to prevent cancer and other chronic diseases among Indigenous people.
- Ontario is home to the largest Indigenous population in Canada, with an estimated 236,680 First Nations,* 120,585 Métis peoples and 3,360 Inuit.[1]
- Rates of cancer, diabetes, heart disease and respiratory diseases are rising in Indigenous peoples.[2] [3]
- First Nations people have more new cases of certain cancers than other people in Ontario.
- Death rates from cancer are also significantly higher in First Nations people than in other people in Ontario.
- Obesity, which raises the risk of developing cancer and other chronic diseases, is markedly more common in Indigenous people than in the general population.[4]
These facts point towards a future of dramatically increased rates of cancer and other chronic diseases among Indigenous people.
For more information about cancer risk factors and screening for Indigenous people, see the following resources:
First Nations People: Cancer Risk Factors and Screening Infographic
Inuit Cancer Risk Factors and Screening Infographic
Metis People: Cancer Risk Factors and Screening Infographic
Beyond cancer
Rates of some other chronic diseases[5] and mental health conditions[6] are also significantly higher in Indigenous people than in the general Ontario population. The death rate for Indigenous people with a chronic disease is far greater as well.[7]
On average, in Canada Indigenous men live 4 years less than non-Indigenous men do. Indigenous women live an average of 6 years less than non-Indigenous women do.[8]
These inequalities can, in part, be explained by determinants of health that disproportionately affect Indigenous people:
- Geographic, financial, cultural and language barriers to accessing care[9]
- Higher rates of risk factors such as:
- commercial tobacco use
- alcohol consumption
- diet (and food insecurity)
- physical inactivity
In addition, Canada's historic policies of colonization – including residential schooling, loss of culture, marginalization and discrimination – have also shaped the health of Indigenous people.
The First Nations, Inuit, Métis and Urban Indigenous Cancer Strategy 2019 – 2023 provides a road map for the Ontario Health (Cancer Care Ontario), Indigenous communities and individuals, and health system partners, will work together to improve health equity and reduce the unique burden of cancer and other chronic diseases on Indigenous people.
This strategy puts forward actions to address cancer care gaps in a holistic approach. It takes into consideration the unique circumstances and needs of Indigenous people living in Ontario, including their distinct sociopolitical, historical and geographical contexts.
FOR MORE INFORMATION
Progress to date
Since 2004, multi-year Indigenous cancer strategies have addressed and led to improvements in cancer care for Indigenous people in Ontario.
This strategy, the fourth, builds on the progress achieved under its predecessors.
The third Aboriginal Cancer Strategy, 2015 – 2019, outlined 41 action items under 6 strategic priorities. Forty of these action items have been completed. Highlights of this work include:
- Building productive relationships: The signing of 10 Relationship Protocols has strengthened relationships between Cancer Care Ontario and Indigenous partners.
- Measurement, monitoring and evaluation: Provincial, regional and community-specific risk factor and cancer burden reports are providing a clearer picture of cancer and factors affecting cancer risk in Indigenous people.
- Prevention: Path to Prevention – Recommendations for Reducing Chronic Disease in First Nations, Inuit and Métis provides evidence-based policy recommendations on 4 key chronic disease risk factors in First Nations, Inuit and Métis communities.
- Screening: The development of community Screening Activity Reports helps healthcare providers in remote communities improve cancer screening rates and appropriate follow-up.
- Palliative and end-of-life care: Cultural competencies embedded into provincial education for service providers is helping to ensure Indigenous patients receive culturally safe palliative care.
- Education: Healthcare professionals are learning about cultural safety, Indigenous history, rights, governance structures and issues, and anti-racism from 13 Indigenous Relationship and Cultural Awareness courses.
About Us
Ontario Health is a new government agency that, once fully established, will be responsible for ensuring Ontarians receive high-quality health care services where and when they need them.
Effective December 2, 2019, Cancer Care Ontario is part of Ontario Health. Cancer Care Ontario’s programs and services, including the work of the Indigenous Cancer Care Unit and Regional Cancer Programs, remain unchanged.
The Indigenous Cancer Care Unit of Ontario Health (Cancer Care Ontario) collaborates with regional, provincial and national Indigenous and non-Indigenous partners and organizations to develop and implement Indigenous cancer strategies. Working together, the Indigenous Cancer Care Unit and Indigenous partners make sure proposed programs and strategies are relevant and have the potential to be highly effective at individual, family and community levels.
The Joint Ontario Indigenous Cancer Committee guides and advises Ontario Health (Cancer Care Ontario) on Indigenous cancer care issues and needs including the development and implementation of the Indigenous cancer strategies . The committee includes representatives from Indigenous organizations and other partners.
Ontario’s 14 Regional Cancer Programs and the Indigenous Cancer Care Unit work closely to understand and serve the unique needs of Indigenous people in each of Ontario’s regions. The Regional Cancer Programs:
- deliver cancer prevention services and care
- make sure standards are met
- listen and respond to local concerns and issues
About this Plan
To create this plan, the Indigenous Cancer Care Unit began by reviewing progress made under third Aboriginal Cancer Strategy 2015 – 2019.
The Joint Ontario Indigenous Cancer Committee, Indigenous patients, families and partners, staff across Cancer Care Ontario and a network of partners, including the Regional Cancer Programs, provided insights and expertise.
The review and engagements confirmed the direction set by previous Indigenous cancer strategies. This strategy continues in the same direction and builds on progress to date. It identifies work that needs to advance, new opportunities for improvement and emerging areas within the healthcare environment that will require attention in coming years.
Acknowledgements
Many individuals and organizations contributed to the development of this strategy. We are grateful for their wisdom and interest in advancing the health of Indigenous people in Ontario.
For more information
Ontario Cancer Plan
The fifth Ontario Cancer Plan is a comprehensive road map that sets out goals, and strategic objectives for improving the provincial cancer system from 2019 to 2023.
Indigenous Tobacco Program
This program works with First Nations, Inuit, Métis and urban Indigenous and non-Indigenous partners to reduce and prevent commercial tobacco addiction.
Indigenous Navigators
Indigenous Navigators provide support and advocacy for First Nations, Inuit, Métis and urban Indigenous patients and families